MYCOBACTERIUM INFECTION
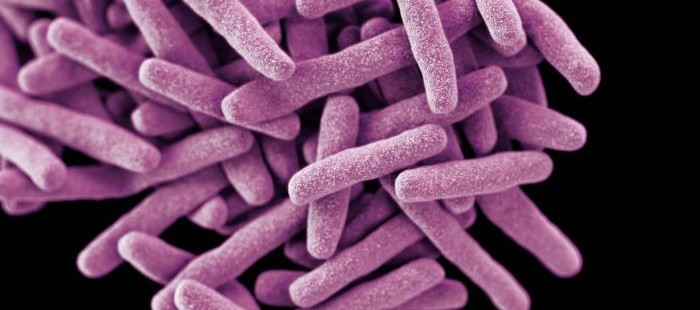
Definition: Mycobacterium is a genus of bacteria includes pathogens known to cause serious diseases, especially in mammals, including tuberculosis. [1]
For the purpose of this discussion, we will consider the species of mycobacterium Mycobacterium tuberculosis, the causative bacteria of pulmonary TB and extrapulmonary TB including cutaneous TB. [2] In specific, we will consider cutaneous TB.
Cutaneous tuberculosis (TB) is an invasion of the skin by Mycobacterium tuberculosis, the same bacteria that causes the better-known TB of the lungs (pulmonary TB). Even in countries such as India and China where TB still commonly occurs, cutaneous outbreaks are rare (<0.1%). [4]
Symptoms
Mycobacteria can colonize their hosts without the hosts showing any adverse signs. For example, billions of people around the world are infected with M. tuberculosis but will never know it because they will not develop symptoms. [3]
Direct infection of the skin or mucous membranes from mycobacteria results in an initial lesion called the tuberculous chancre. [4] The chancres are firm shallow ulcers with a granular base. They appear about 2-4 weeks after mycobacteria enter through broken skin and the immune response of the patient and the virulence of the mycobacteria determines the type and severity of cutaneous TB. [4]
Types of TB
TB verrucosa cutis – This occurs after direct inoculation of TB into the skin in someone who has been previously infected with mycobacteria, and appears as a purplish or brownish-red warty growth. [4] Lesions associated with this type of TB may persist for years but can clear up even without treatment. [4]
Lupus vulgaris – This is a persistent, progressively worsening form of cutaneous TB that presents as small sharply defined reddish-brown lesions with a gelatinous consistency (called apple-jelly nodules). [4] These lesions can worsen or persist for years. [4]
Scrofuloderma – This disease usually presents with skin lesions that result from direct extension of underlying TB infection of lymph nodes, bone or joints. It is often associated with TB of the lungs. [4] Infected patients have firm, painless lesions that eventually ulcerate with a granular base. These may heal without treatment, but often these lesions leave scars. [4]
Military TB – This is a chronic TB infection that has spread from the primary infection (usually in the lungs) to other organs and tissues via the bloodstream. [4] It results in skin lesions that are small (millet-sized) red spots that develop into ulcers and abscesses. This occurs more frequently in immunocompromised patients, and prognosis is poor. [4]
Diagnosis
The diagnosis of typical TB of the lungs is performed through sputum culture and acid fast staining. The reason for the acid-fast staining is because of the mycobacteria thick, waxy cell wall. [5]
The diagnosis of TB in a patient with skin lesions is usually made or confirmed by a skin biopsy. [4] Other tests that may be necessary include:
- Tuberculin skin test (Mantoux)
- Quantiferon-Gold blood test
- Sputum culture (it may take a month or longer for results to be reported)
- A Chest X-ray or other imaging for sites of infection outside the lung [4]
Treatment
Mycobacterial infections are notoriously difficult to treat. The organisms are hardy due to their cell wall, which is naturally resistant to a number of antibiotics that work by destroying cell walls, such as penicillin. Mycobacteria are neither truly Gram negative nor gram positive. [3] Due to the waxy cell wall, they can survive long exposure to harsh chemicals, detergents, oxidative burst, and antibiotics, which naturally leads to antibiotic resistance. Most mycobacteria are susceptible to the antibiotics clarithromycin and rifamycin, but antibiotic-resistant strains are known to exist. [3]
Patients with pulmonary or extrapulmonary (outside the lung) TB diseases need to be treated with antitubercular drugs. This usually involves a combination of antibiotics (isoniazid, rifampicin, pyrazinamide and ethambutol) given over a period of several months and sometimes years. [4] It is important that patients diagnosed with TB finish the entire course of antibiotics prescribed. Patients with TB infection but no active disease must also be treated with antitubercular drugs to prevent development of active disease. [4]
Occasionally surgical excision of localized cutaneous TB is recommended. [4]
References
- Ryan KJ, Ray CG (editors) (2004). Sherris Medical Microbiology (4th ed.). McGraw Hill.
- McCann et al. (2009). “Secreted and Exported Proteins Important to Mycobacterium tuberculosis Pathogenesis”. Bacterial Secreted Proteins: Secretory Mechanisms and Role in Pathogenesis. Caister Academic Press.
- Madigan M, Martinko J (editors) (2005). Brock Biology of Microorganisms (11th ed.). Prentice Hall.


